Detailed Review of the Maskin® Protocol for Meibomian Gland Probing
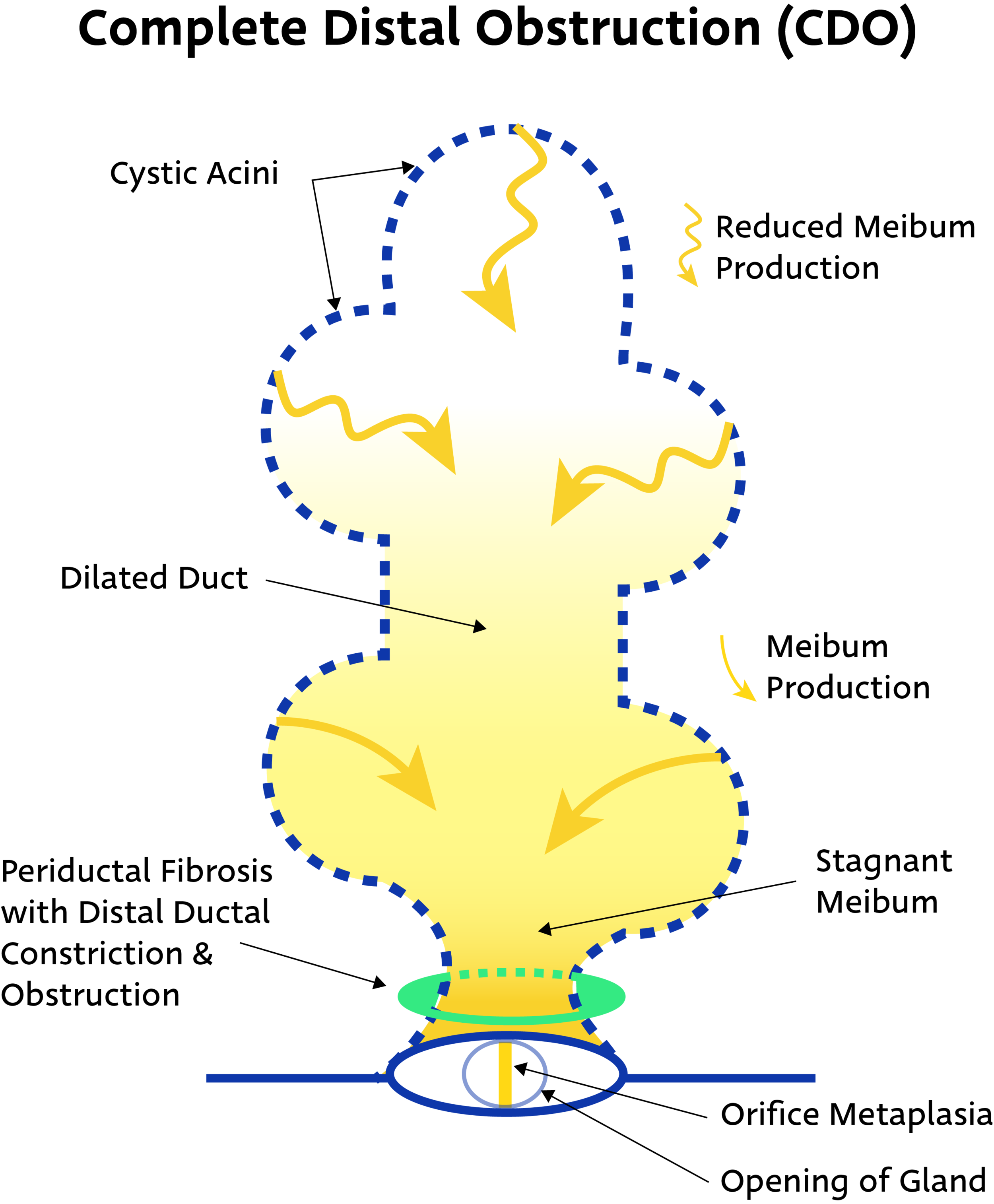
Meibomian Gland Probing is a simple and effective procedure to release periductal fibroses from Meibomian Glands, freeing glands from strictures that block the flow of indispensable meibum.
It is essential to treat co-morbid diseases (such as aqueous tear deficiency, allergy, and anterior blepharitis). Without sufficient and thorough treatment for root causes of dry eye, patient will have a significant reduction in benefit duration and require probing repetition more quickly. Annual probing is recommended for maintenance as Meibomian Gland disease progresses in a subclinical manner.
Tips for Patient Care during the Probing Procedure:
Discuss the indicators for probing and how periductal fibroses (scar tissue) around the gland constricts to create blockages.
MGDi recommends using gland images (available for download) to illustrate strictures at different points along the gland length, leading to differential functional ability of glands and progressive gland atrophy.
Review resultant symptoms, such as lid tenderness (LT), burning, and sensitivity to light (photophobia).
Share the number of functional glands both pre-probing and in post-probing follow up visits so the patient is aware of her starting point and progress.
Let the patient know the procedure in its entirety prior to beginning. Share how many glands you expect to probe, which lid(s), and if you plan to use multiple probe lengths.
Allow the patient to spread the probing procedure over a few days or weeks, instead of doing all 4 lids at once.
Explain sensations the patient may feel throughout the procedure.
For example, let the patient know she may feel mild burning immediately after jojoba anesthetic ointment is applied to the lids, but it should dissipate in 60 secs.
Inform the patient the procedure may be uncomfortable but is not painful with sufficient anesthetic. Instruct the patient to ask for more anesthetic if feeling pain during the procedure.
Remind the patient she may feel or hear a popping or several pops in a gland as it is probed. As bands of scar tissue are released, the equilibration of pressure and release of constriction may be detectable in this way.
Try to give patients the big picture of short- and long-term results of probing.
Explain the role of co-morbid disease in gland health, what comorbidities they have, and the expected timeline for treatment.
Remind patients glands will become occluded once again and more rapidly if co-morbid disease not treated adequately.
Prepping for Meibomian Gland Probing:
Evaluate patency of orifice, gland proximal and distal atrophy, gland length, and ductal dilation using slit lamp with trans-illumination and/or meibography.
Palpate glands individually to evaluate tenderness and number of expressible glands.
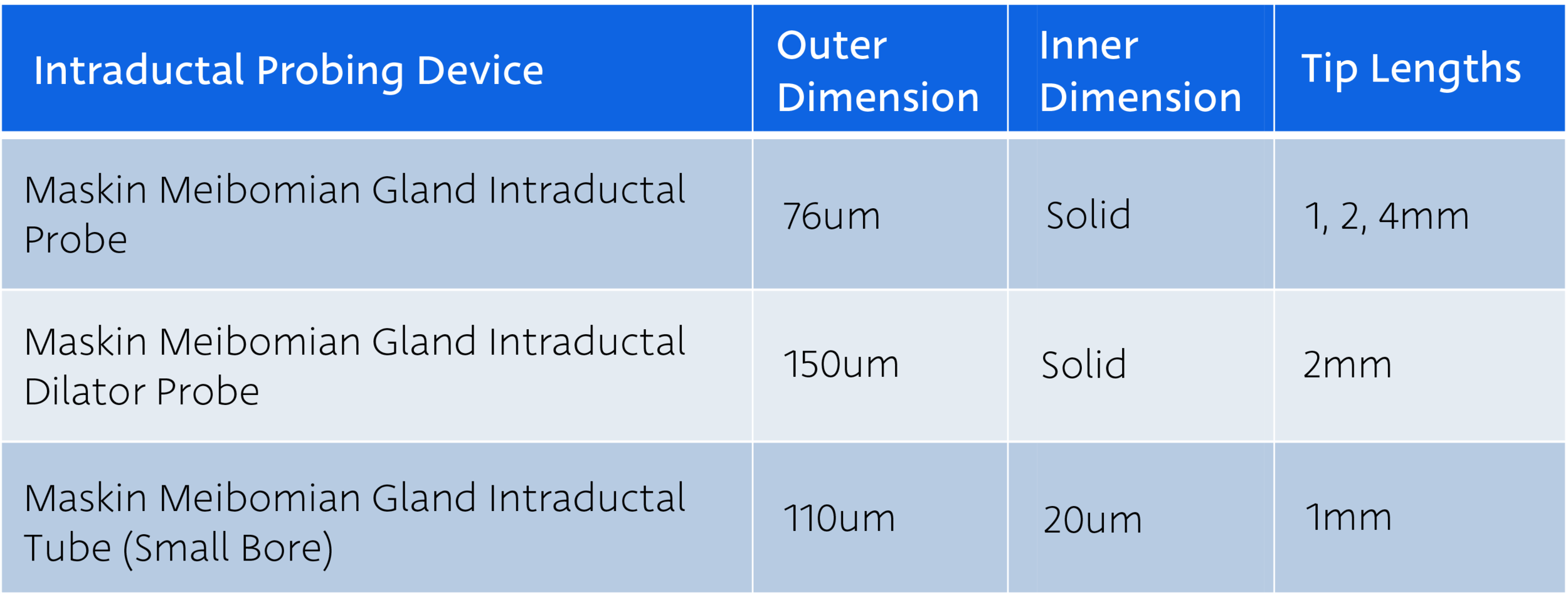
Confirm multiple probes of each length are available for the procedure, as well as any tube or dilator products (items reviewed below).
While infrequent, probes occasionally bend or become misshapen during the probing procedure due to heavy scarring around glands. If this happens, switch out the probe for a new version of the same length.
Be sure to start probing with the shortest and stiffest probe, 1mm, to most efficiently and effectively clear scarring from around Meibomian Glands.
Refrigerate jojoba anesthetic ointment until use. Upon completion of procedure, return to refrigerator. Ointment loses potency roughly 2 months after purchase.
If probing at slit lamp, designate a team member to place a hand lightly but firmly behind the patient’s head to hold it steady throughout the procedure.
Maskin® Protocol for Meibomian Gland Probing Procedure:
Put 1 drop of proparacaine 0.5% or tetracaine 0.5% solution in the conjunctival sac.
Place bandage contact lens.
Distribute a generous amount of jojoba ophthalmic anesthetic ointment (about the size of a marble) on lower lid margin using sterile cotton-tipped applicator. Application should be abundant enough to visibly coat the lower lid margin with a thick layer of anesthetic.
Patient closes lids 10 minutes. Burning from ointment dissipates over 60 secs.
If numbing is insufficient for patient comfort, repeat application.
After 10 minutes, place an additional drop of topical anesthetic solution in the conjunctival sac to eliminate possible mild burning when eyes are opened.
Begin probing with the shortest and stiffest probe, the 1 mm length.
Seat probe tip on the orifice then advance through with a dart-like motion.
Adjust location and angle of probe to find proper entry position, especially in cases of cicatricial MGD.
For difficult or occult orifices, use slit lamp red free light or transilluminate lid.
When resistance is encountered, confirm probe is co-linear to the gland then use mild additional force to pop through internal lumen strictures, similar to popping a thin lacrimal punctal scar.
Use longer probes (2mm, 4mm) if persistent LT suggests deeper obstruction.
Expression may be performed using Maskin® Meibum Expressor or other method.
MGDi does not recommend placing excessive direct pressure on lid for expression.
Inject therapeutic into glands using Maskin® Intraductal Microtube, if indicated. See MG Injection Guide for additional detail.
Remove bandage contact lens.
Rinse eye copiously with sterile preservative-free saline and use cotton-tipped applicator to remove all residual anesthetic from lid margin and lashes.
Give patient preservative-free artificial tears to use every hour until bedtime.