Research
many eye doctors continue to investigate meibomian gland probing (MGP) and its impact on eye health.
We’ve collected and made available the results of this research for your continued education. Select the plus sign (+) next to the reference listing to see additional details from the study.
Dry Eye Definition and Prevalence:
+ 1. Craig JP, et al., TFOS DEWS II Report Executive Summary, The Ocular Surface (2017), http: //dx.doi.org/10.1016/ j.jtos.2017.08.003. (PDF for Download)
- Dry eye is one of the most frequent causes of patient visits to eye care practitioners. It is a symptomatic disease, characterized by a vicious cycle of tear film instability and hyperosmolarity, which leads to increased ocular surface inflammation, damage and neurosensory abnormalities. Moderate to severe DED is associated with significant pain, limitations in performing daily activities, reduced vitality, poor general health, and often depression.
- Age, sex, race, MGD, connective tissue disease, Sjogren syndrome, androgen deficiency, computer use, contact lens wear, estrogen replacement therapy, hematopoietic stem cell transplantation, certain environmental conditions (such as pollution, low humidity, and sick building syndrome) and medication use (for example, antihistamines, antidepressants, anxiolytics, and isotretinoin) were identified as consistent risk factors.
- Probable risk factors included diabetes, rosacea, viral infection, thyroid disease, psychiatric conditions, pterygium, low fatty acid intake, refractive surgery, allergic conjunctivitis, and additional medications (e.g. anti-cholinergic, diuretics, b-blockers).
- Affects 30 million in the US alone and at least 344 million worldwide. (Report Summary Page)
+ 2. Lemp MA, Crews LA, Bron AJ et al. Distribution of aqueous-deficient and evaporative dry eye in clinic-based patient cohort: A retrospective study. Cornea 2012; 31:472-478. (Abstract)
MGD is the most common cause of dry eye in the world, seen in 86% of dry eye patients.
+ 3. Kelly K. Nichols; Gary N. Foulks et al. The International Workshop on Meibomian Gland Dysfunction: Executive Summary. Investigative Ophthalmology & Visual Science March 2011, Vol.52, 1922-1929. doi:10.1167/iovs.10-6997a (PDF for Download)
- Meibomian gland dysfunction (MGD) is a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/ or qualitative/ quantitative changes in the glandular secretion.
- MGD results in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease.
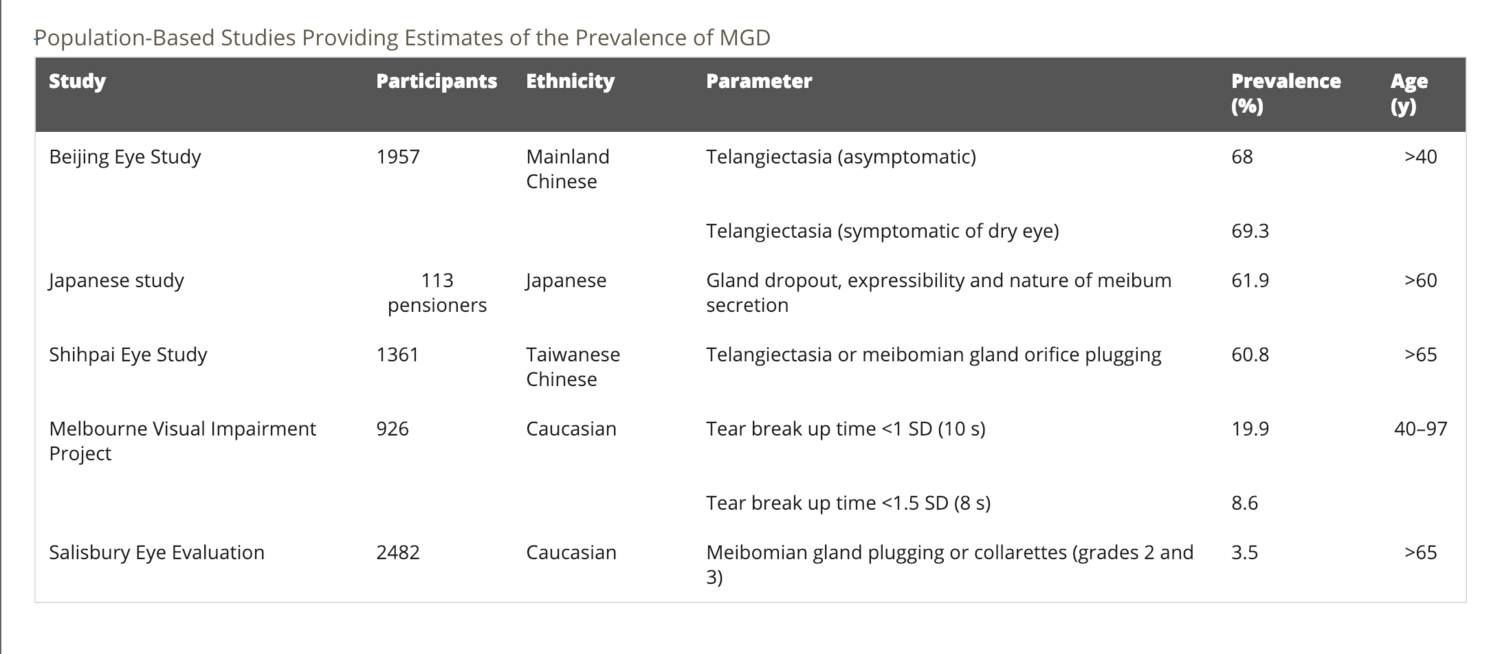
- Reported prevalence of MGD varies widely, and appears to be higher in Asian populations, reported as > 60% in different Asian population-based studies. Current research on MGD prevalence in Caucasians varies from 3.5%-19.9%.
Meibomian Gland Probing
1. Maskin, SL, Toland, C. Intraductal Meibomian Gland Probing (MGP) Leads to More Superficial and Accelerated Meibomian Gland (MG) Basement Membrane (BM) Differentiation with Increased Ductal Epithelial Cell Layers (ECL). Poster presented at World Cornea Congress 2022, Chicago.
2. Maskin, SL. Successful reversal of neuropathic eye pain by treatment of occult ocular surface disease: Case series and implications. American Journal of Ophthalmology Case Reports, 2022: 101662. (Full text available online)
3. Maskin, SL. Rete Ridge Structures Form Meibomian Gland Distal External Duct Wall and Basal Epithelial Layer. Investigative Ophthalmology & Visual Science 63.7 (2022): 1967-A0297. Poster presented at ARVO 2022, New Orleans.
4. Maskin, Steven L with Warren, Natalia A. Your Dry Eye Mystery Solved: Reversing Meibomian Gland Dysfunction, Restoring Hope. Yale University Press, 2022. (Purchase from Yale University Press or Amazon)
5. Maskin, Steven L. Comments on: Intraductal Meibomian Gland Probing and its Efficacy in the Treatment of Meibomian Gland Dysfunction. Survey of Ophthalmology 66.4 (2021): 680-685. (Full text available online)00059-X/fulltext)
6. Maskin SL, Alluri, S. Intraductal meibomian gland probing (MGP) leads to ductal epithelial proliferation with increased duct wall thickness. Investigative Ophthalmology & Visual Science 61.7 (2020): 96-96. Abstract presented at ARVO 2020, Baltimore.
7. Maskin, SL, Alluri, S. An Alternative Hypothesis of Atrophic Meibomian Gland Dysfunction Using Stem Cell Concept. Investigative Ophthalmology & Visual Science 61.7 (2020): 343-343. Abstract presented at ARVO 2020, Baltimore. (Abstract available online)
8. Maskin SL, Alluri S., Meibography Guided Intraductal Meibomian Gland Probing Using Real-Time Infrared Video Feed, British Journal of Ophthalmology. Published Online First: 27 February 2020. doi: 10.1136/bjophthalmol-2019-315384, (Full text available online)
9. Maskin SL, Alluri S., Expressible Meibomian Glands Have Occult Fixed Obstructions, Cornea 2019:38 880-887, (Full text available online)
10. Maskin SL, Alluri S., Intraductal meibomian gland probing: background, patient selection, procedure, and perspectives, Clinical Ophthalmology 2019:13 1203-1223, (Access article and video)
11. Nirupama D, Hymavathi B, Prathima L, et al. Meibomian gland probing in patients with meibomian gland dysfunction. Indian Journal of Clinical and Experimental Ophthalmology. 2019;5(1):78–81. (PDF for Download)
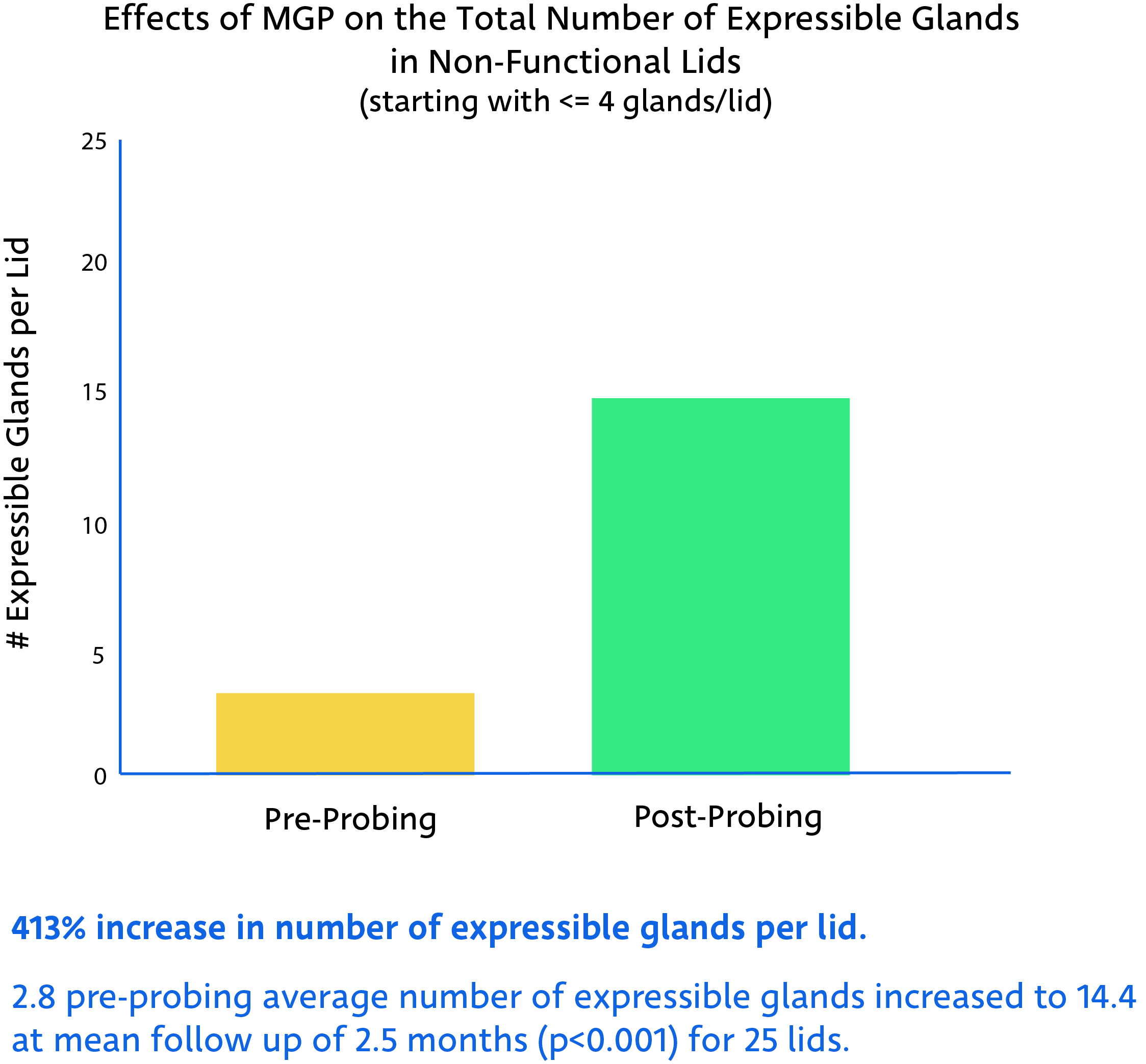
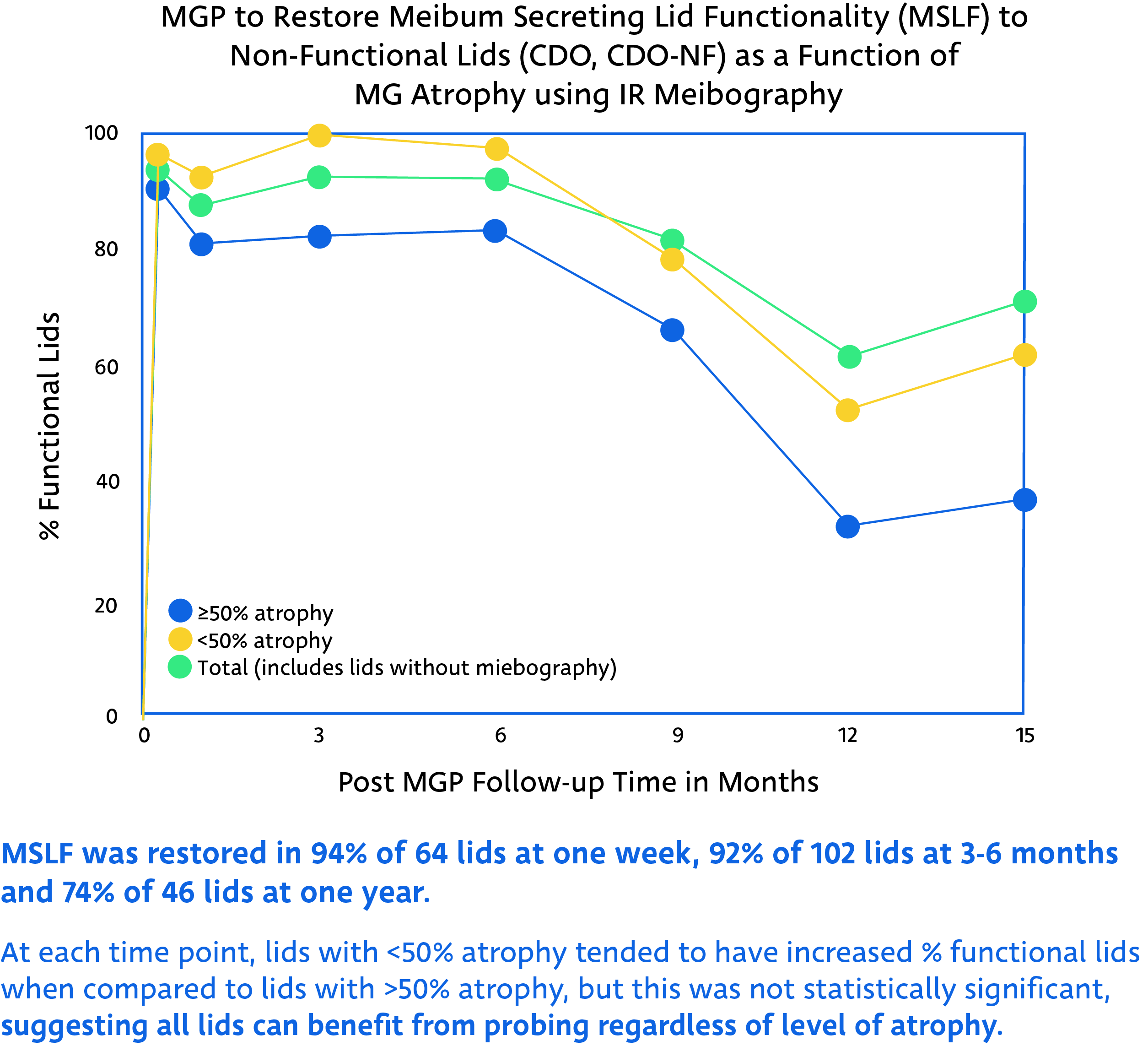
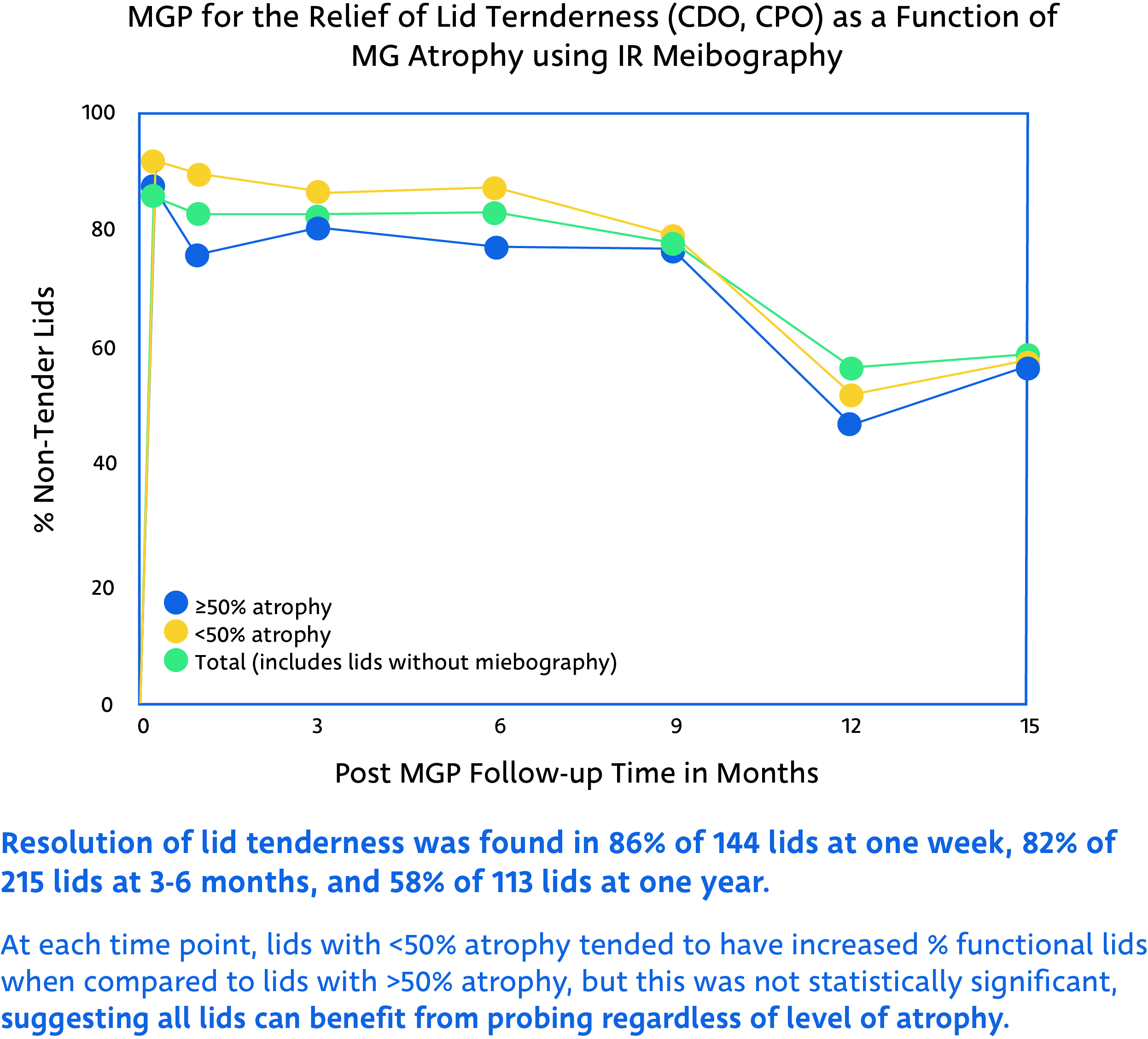
+ 12. Maskin SL, Testa WR Growth of meibomian gland tissue after intraductal meibomian gland probing in patients with obstructive Meibomian gland dysfunction. British Journal of Ophthalmology. 2018;102:59-68 (PDF for Download)
- Scarring around gland develops in setting with presence of:
- Local disease, which causes ocular surface or lid inflammation
- Regional or systemic disease associated with periglandular inflammation
- Study Results:
- Within 1 week, dramatic resolution of lid tenderness in 86% of cases
- Return of meibum secreting lid functionality (5 or more expressible gland per lid) in 94% of cases
- Increase in number of expressible glands by 412% (p<0.001)
- Post-MGP meibography of 34 lids showed 41.2% with MG growth, including lengthening of shortened glands (reversing proximal atrophy), partial restoration of faded glands, and appearance of a new gland.
+ 13. Maskin SL, Meibomian Gland Probing (MGP): Safely Providing Outflow Patency with Positive Physical Proof: Concepts, Literature Review and Results. AAO Instructional Course 2018, Chicago.
14. Incekalan TK, Harbiyeli II, Yagmur M, Erdem E. Effectiveness of intraductal meibomian gland probing in addition to the conventional treatment in patients with obstructive meibomian gland dysfunction AU - Incekalan, Tuğba Kurumoglu. Ocul Immunol Inflamm. Epub 2018 Sep 20. (Abstract)
+ 15. Cardenas Diaz, Guerra Almaguer, Hernandez Lopez et al: Efficacy of intraductal probing in Meibomian Gland dysfunction. Revista Cubana de Oftalmologie. 2017; 30(2): 1-12 (Full text available online)
- Cuban prospective longitudinal study of 50 eyes in 25 patients
- Improvement in tear breakup times (TBUT), reduction in artificial tear usage and ocular surface disease (OSDI) at 1 and 6 months (p<0.001).
+ 16. Syed ZA, Sutula FC. Dynamic intraductal meibomian probing: A modified approach to treatment of obstructive Meibomian gland dysfunction. Ophthal Plast Reconstr Surg. 2017; Jul/Aug;33(4):307-309. (Abstract)
- Study from Massachusetts Eye and Ear Institute showed effects of probing on 70 lids in 41 patients
- 92% of cases experienced symptomatic improvement within 1 week of probing with no complications during follow-up (average 3.5 months)
+ 17. Hamrah et al: A randomized sham-controlled trial of intraglandular meibomian gland probing for obstructive Meibomian gland dysfunction. Poster presented at AAO 2016, Chicago.
- Independent prospective double blinded randomized controlled trial to compare MG probing with sham probing.
- Showed statistically significant improved symptoms for probed patients in Symptom Assessment in Dry Eye (p<0.007) and OSDI (p=0.02), as well as signed of reduced telangiectasia (vascular lesions) (p=0.04).
+ 18. Ma X et al: Efficacy of intraductal meibomian gland probing on tear function in patients with obstructive meibomian gland dysfunction. Cornea 2016 35: 725-30. (Abstract)
- Evaluated efficacy and safety of probing in 49 patients with obstructive MGD that had been unresponsive to treatment. Patients were randomized into 2 groups: steroid treatment alone and steroid treatment with probing.
- Before applying any medications, 76% of patients relieved immediate symptom relief 1 day after probing.
- Probing group also showed statistically significant improvements to meibum grade (p<0.001), lid margin abnormalities (p<0.001), and tear break up times (p=0.029) when compared to steroid only group.
19. Maskin SL. Intraductal meibomian Gland Probing: A paradigm shift for the successful treatment of obstructive meibomian gland dysfunction. In: Kazuo Tsubota, ed. Diagnosis and Treatment of Meibomian Gland Dysfunction. Tokyo, Japan: Kanehara;2016:149-167
+ 20. Sik Sarman Z et al: Effectiveness of intraductal meibomian gland probing for obstructive meibomian gland dysfunction. Cornea 2016 35: 721-4 (Abstract)
- Prospective study of 58 eyes of 30 MGD patients resistant to therapy for at least 6 months.
- Tear breakup time increased from 5 seconds to 13 seconds at 3 months post probing (p<0.001).
- Also showed statistically significant decreases in conjunctival hyperemia (p<0.001) and eye margin vascularization (p=0.004), as well as significant improvement in Ocular Surface Disease Index (OSDI) at 3 months.
+ 21. Fermon S, Hindi Zaga I, Alvarez Melloni D: Intraductal meibomian gland probing for the treatment of blepharitis. Arch Soc Esp Oftalmol Epub: 2015; 90:76-80 (Abstract)
Prospective longitudinal study showed a statistically significant improvement in treated eye of 16 patients for TBUT (p<0.001), visual acuity (p<0.001), level of pain (p=0.008), and photophobia (p<0.001) when compared to untreated eye.
+ 22. Maskin SL, Hethorn WR. Meibomian Gland Probing (MGP) for Lid Tenderness (LT) & Non-Functioning Meibomian Glands in Meibomian Gland Dysfunction (MGD), presented at AAO 2015, Las Vegas.
+ 23. Nakayama N et al: Analysis of meibum before and after intraductal meibomian gland probing in eyes with obstructive Meibomian gland dysfunction. Corner 2015 34: 1206-8 (Abstract)
- Study from Japan of 6 eyelids on 3 patients.
- All cases showed improvement in meibum lipid level and meibum viscosity at 1 month post probing and ⅔ showed improvement in TBUT.
- No morphological changes in Meibomian glands using infrared meibography analysis.
+ 24. Dongju Q, Hui L, Jianjiang X. Clinical research on intraductal meibomian gland probing in the treatment of patients with meibomian gland dysfunction. Chin K Optom Ophthalmol. 2014; 16(10):615-21
- Prospective randomized study over 1 month examined 111 age and sex matched patients over 1 month to compare MGP with and without steroid injection to conventional treatment (eyelid hygiene with topical/steroid/artificial tear drops).
- Saw statistically significant improvement of both MGP groups in OSDI, TBUT, cornea fluorescein staining, Schirmer 1 test, and lid margin scores (p<0.05).
- Confocal microscopy showed no post probing degenerative changes in morphology to MG acinar units or MG scars.
+ 25. Mickles C et al: Unplugged: A comparison of intraductal meibomian gland probing and conventional meibomian gland dysfunction treatment. Presented at American Academy of Optometry annual meeting Denver, CO, 2014
Showed significant improvement in outcome measures when compared to conventional lid hygiene therapy, including improved TBUT (p=0.02) and meibum quality (p=0.03).
+ 26. Narayanan S et al: Evaporative dry eye treatment with Retaine MGD artificial tears or intraductal meibomian gland probing a comparison. Presented at American Academy of Optometry annual meeting Denver, CO, 2014. (Abstract)
Showed significant improvement in outcome measures when compared to lipid containing artificial tears, including improved OSDI (p<0.01) and TBUT (p<0.05).
+ 27. Yagmur M et al: Effectiveness of intraductal meibomian gland probing for the management of obstructive meibomian gland dysfunction. Poster presented at ESCRS 2014, London. (Abstract)
Showed statistically significant rapid relief of symptoms evaluated by OSDI, TBUT, Schirmer’s test, and meibum score when compared to control eyes (p<0.001).
+ 28. Maskin SL. Meibomian gland probing findings suggest fibrotic obstruction is a major cause of obstructive meibomian gland dysfunction (o-mgd). Investigative Ophthalmology & Visual Science. 2012;53(14):605. (Abstract)
- FFFUR (fixed, firm, focal, unyielding, resistance) found in 74% of upper and 55% of lower lid MGs.
- This type of resistance represents periductal fibroses (scar tissue) contracting around the gland duct, leading to compromise and strictures and associated partial or complete obstruction of meibum flow.
29. Maskin SL et al: Meibomian gland probing findings suggest fibrotic obstruction is a major cause of obstruction for meibomian gland dysfunction (O-MGD). Poster presented at ARVO 2012, Ft. Lauderdale, FL (PDF for Download)
+ 30. Wladis E: Intraductal meibomian gland probing in the management of ocular rosacea. Ophthal Plast Reconstr Surg 2012 28: 416-8 (Abstract)
- 40 lids of 10 patients.
- Showed a statistically significant improvement post probing in OSDI scores at 1 and 6 months post-probing.
- All patients reported decreased use of artificial tears (p<0.05)
- No adverse effects of probing seen.
31. Knop E, Knop N, Millar T et al. The international workshop on Meibomian gland dysfunction: Report of the subcommittee on anatomy, physiology and pathophysiology of the Meibomian gland. Investigative Ophthalmology and Visual Science 2011;52:1938-1978 (PDF for Download)
32. Maskin SL, Kantor K. Intraductal meibomian gland probing with adjunctive intraductal microtube steroid injection (MGPs) for meibomian gland dysfunction (MGD). Investigative Ophthalmology and Visual Science 2011;52.1 (Abstract)
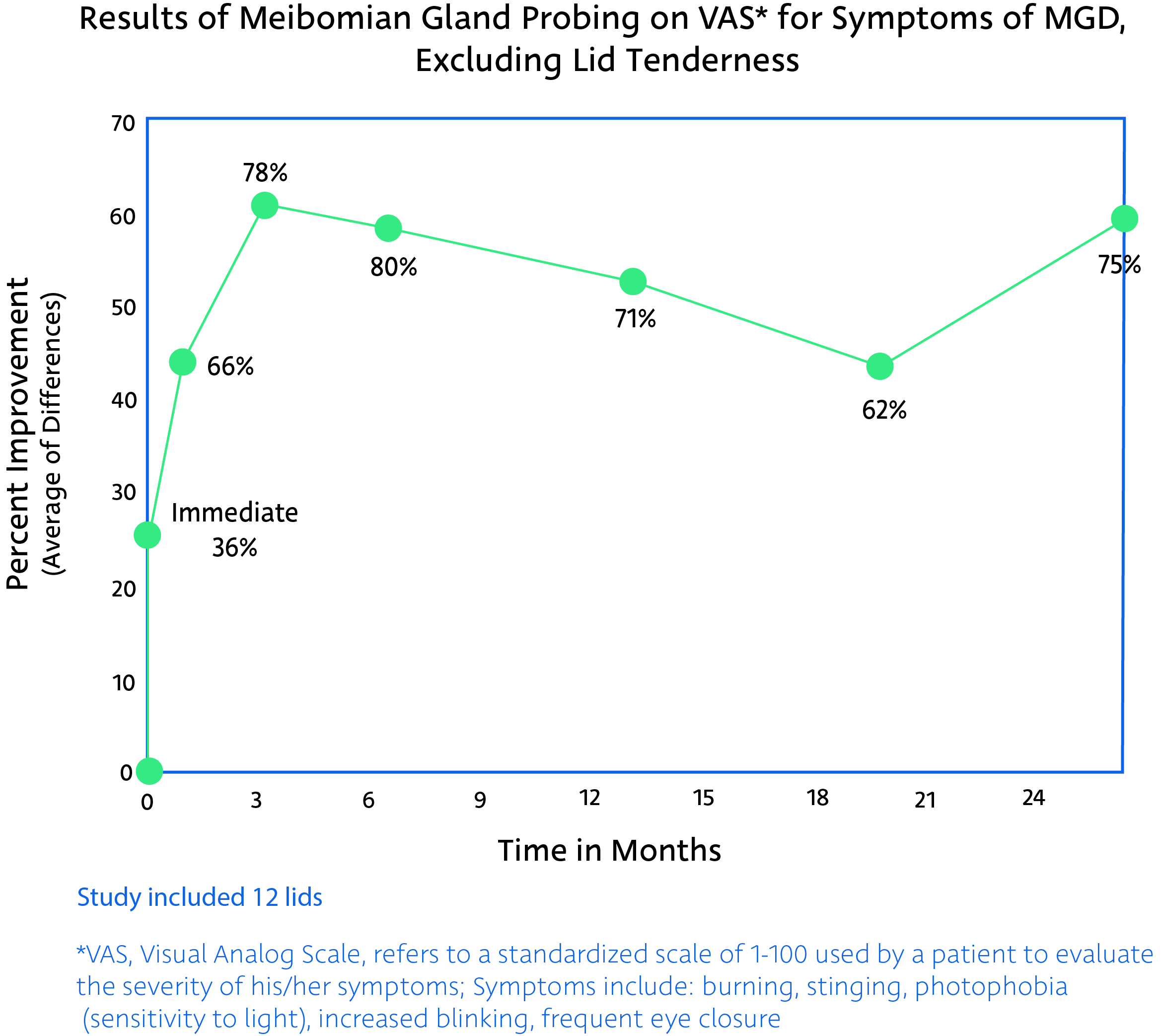
+ 33. Maskin SL: Intraductal Meibomian gland probing to restore gland functionality for obstructive Meibomian gland dysfunction. Poster presented at AAO 2011, Orlando, FL (PDF for Download)
34. Maskin SL, Kantor K.: Intraductal Meibomian Gland Probing for Meibomian Gland Dysfunction Using VAS Testing. Poster presented at AAO 2010, Tampa, FL. (PDF for Download)
35. Maskin SL: Intraductal Meibomian gland probing relieves symptoms of obstructive Meibomian gland dysfunction. Cornea. 2010;29(10):1145-52 (Abstract)
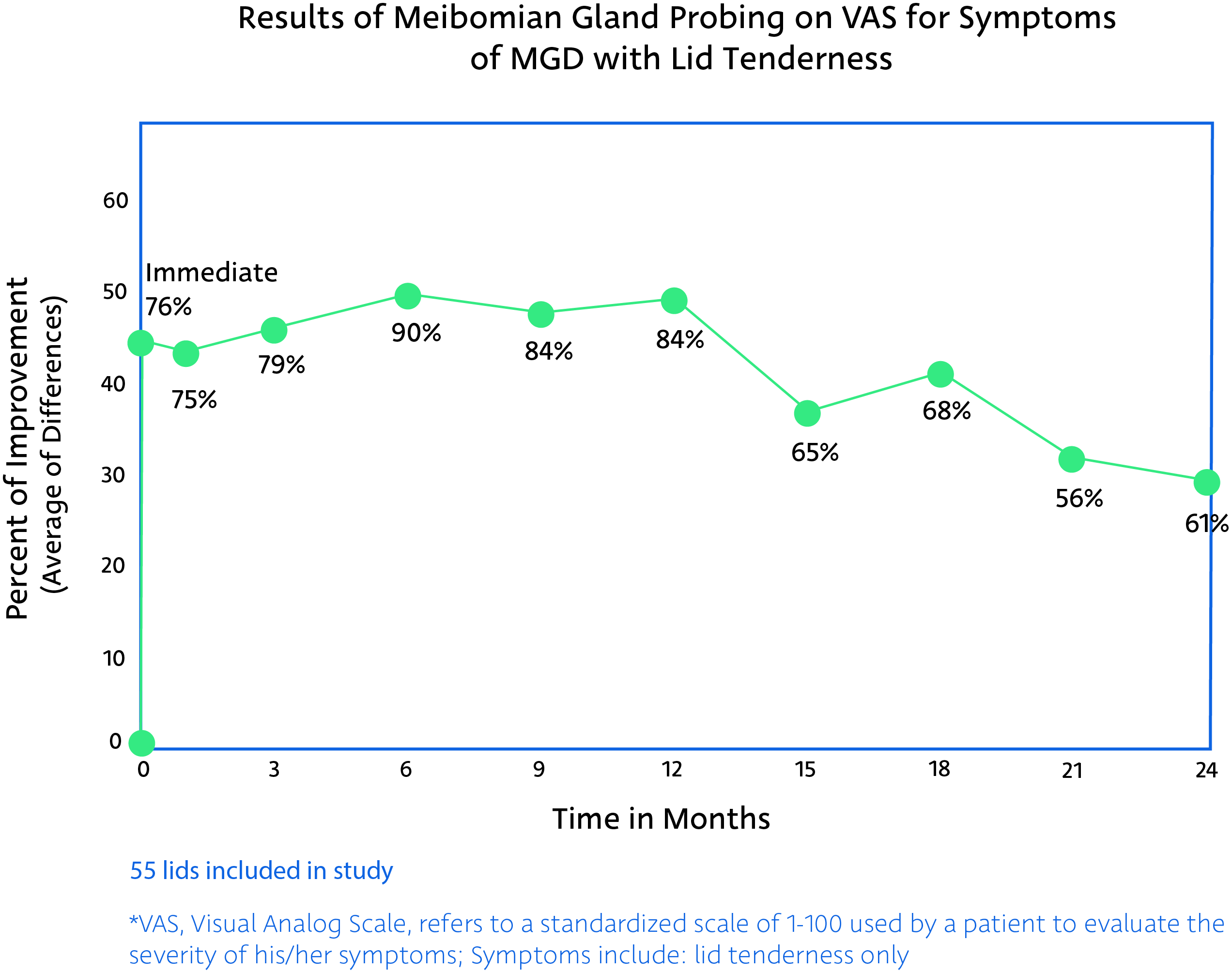
+ 36. Maskin SL: Intraductal meibomian gland probing and distinct visual analog scale response profiles for symptoms of Meibomian gland dysfunction. Poster presented at AAO 2010, Chicago, IL
MG probing results in >75% reduction in severity of symptoms